About Giant Cell Arteritis
Giant cell arteritis (GCA) is a chronic systemic vasculitis of medium and large sized arteritis (includes aorta and its branches).
- Most common vasculitis in people >50 yo
- Incidence increases with age
- 10x more common in patients in their 80s than those in their 50s-60s
- Temporal arteritis can be a manifestation of giant cell arteritis, but this form of vasculitis may also involve large arteries such as the aorta, carotid, and subclavian arteries.
- Requires immediate treatment with high-dose glucocorticoids due to risk of blindness
- 40-60% of patients with GCA have polymyalgia rheumatica (PMR) symptoms, while 15-20% of patients with PMR will develop GCA.
- Important to screen for GCA signs and symptoms in a patient with PMR!
- Increased risk of thoracic aortic aneurysm (TAA) even 5+ years after diagnosis
Incidence
- 2-3x more common in women
- Although more common in caucasians of Northern European descent, GCA has been described in individuals of ALL ethnicities and races.
Temporal Artery Abnormalities & Scalp Tenderness
- Tenderness
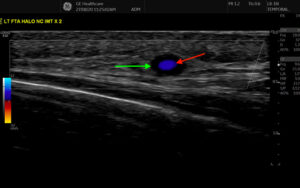
- Loss of temporal artery pulsation is common (view image)
Constitutional
- Weight loss
- Low grade fever
- Fatigue
- Night sweats
Visual
- Amaurosis fugax (transient vision loss)
- Acute visual loss
- Visual loss occurs in 15% of patients (MC due to ischemic neuritis)
- Blindness is abrupt and painless
- Diplopia
PMR
- Significant stiffness that’s predominant in the morning and improves with activity
- Affecting the neck, shoulders, and pelvic girdle
Large Vessel Vasculitis
- Asymmetric BP in upper limbs
- Jaw and/or tongue claudication, limb claudication
Biopsy
- Temporal artery biopsy is the gold standard.
- Biopsy often shows findings of arteritis even after more than 14 days of steroid therapy.
- Ideally obtained within 14 days of starting steroids, although positive biopsy may be seen for several months
- Need about 1.5-2 cm length of tissue, as skip lesions can occur
Imaging
- Ultrasound of temporal artery – halo sign is consistent with GCA (view image) but dependent on skill of ultrasonographer
- MRA, CTA, or PET-CT may identify large vessel vasculitis lesions.
Lab Workup
- Other vasculitides
- Takayasu arteritis
- Also affects aorta and primary branches, but typically under 40 yo and F
- Granulomatosis with polyangiitis (GPA)
- Polyarteritis nodosa (PAN)
- Microscopic polyangiitis (MPA)
- Takayasu arteritis
- Ischemic vascular disease, ischemic optic neuropathy, retinal artery/vein occlusion, migraine headaches, TMJ OA, dental disease
- Other causes of headache
- Other causes of vision loss
- Malignancies (especially in patients with elevated inflammatory markers)
Glucocorticoid Therapy
- Initial dosing 1 mg/kg daily in divided doses
- Do not delay by waiting to confirm by biopsy or imaging if clinical suspicion is high, especially in the setting of threatened or acute vision loss
- If threat of acute visual loss at diagnosis, should be treated with IV methylprednisolone 1 g daily X 3 days
- High dose therapy is usually continued for 1 month or until ESR/CRP normalize and then is tapered slowly
- Taper can last 6 months-2 years
Aspirin
- Aspirin may be added for GCA patients with critical or flow-limiting involvement of the vertebral or carotid arteries.
Adjunctive Immunosuppressive Therapy
- Consult rheumatology to consider start of tocilizumab (anti-IL6) for any new or relapsing GCA patient, if no contraindications
Bone Health
- Treat to prevent glucocorticoid-induced osteoporosis, given need for long-term steroids
Exercise and Nutrition Counseling
- To prevent falls, steroid myopathy and frailty
- Regular follow-up every 3 months
- Monitor based on symptoms:
- Worsening headaches
- Increased temporal artery tenderness
- Scalp tenderness
- Jaw/tongue claudication
- PMR symptoms
- Monitor for signs of AAA or TAA
- Needs to be urgently evaluated in a GCA patient
- Yearly abdominal ultrasound should be considered
- Monitor with ESR and CRP (which should decrease and normalize with treatment)
- Very important to monitor for steroid complications for patients with GCA (steroid-induced osteoporosis is very common early on in steroid therapy)
Clinical Presentation
- GCA is most common among 70-80 yo, although younger or older presentation is possible.
- Jaw claudication, fatigue after chewing for several minutes, is a highly specific symptom for GCA.
- Jaw pain that starts upon opening/closing mouth is more indicative of TMJ OA/pain.
- Evaluate for signs and symptoms of GCA in a patient with symptoms of PMR (morning stiffness affecting neck, shoulders, pelvic girdle)
Diagnostic Workup
- Ultrasound has utility (halo sign indicates temporal arteritis – view image), but it is very operator dependent.
- Although possible, GCA rarely presents with normal inflammatory markers.
- Temporal artery biopsy can yield diagnosis/show inflammation even 2 weeks after steroid start.
Treatment & Monitoring
- Treatment should not be delayed for diagnostic purposes, as vision loss is a concerning complication.
- Mainstay of therapy: systemic steroids and IL6 axis inhibitors
- Very important to monitor for steroid complications
- Steroid-induced osteoporosis is very common early on in steroid therapy.