About Sjogren’s Disease
Sjogren’s is a chronic, inflammatory autoimmune disease involving exocrine gland inflammation.
- Extra-glandular symptoms affect up to 40% of pts
- F:M = 9:1
- Peak age 50-60 yo
Generally presents with inflammation of exocrine glands +/- extraglandular features.
Sjogren’s can present as a primary disease called Sjogren’s disease, in the absence of another underlying disease, or a patient can have secondary Sjogren’s. In secondary Sjogren’s, patients have the symptom of dry mouth (xerostomia) and/or dry eyes (xerophthalmia), associated with another underlying rheumatic disease (rheumatoid arthritis, lupus, systemic sclerosis, etc.)
- Most common symption: sicca = dry eyes and/or dry mouth in >85% pts
- Ocular:
- Predominant dryness in the morning
- Dry and itchy feeling
- Foreign body/gritty sensation
- Eye redness
- Dry mouth → frequent cavities (view image)
- Inability to eat dry food (bread, crackers, etc.)
- Difficult speaking for long period due to dryness
- Mouth burning
- Parotid gland enlargement (view image)
- Extraglandular features:
- Arthritis in up to 45%, arthralgia more common
- Neuropathy: PNS in up to 35%
- Renal and GU: RTA IV (hypokalemia, acidosis), interstitial cystitis, vaginal dryness
- Pulmonary: rarely lymphocytic interstitial pneumonitis (LIP)
- Cardiac: pericarditis, pulmonary hypertension
- GI
- Rash
- Raynaud’s phenomenon
- Cytopenias
- Dysautonomia
Lab workup
- SSa/SSb+ in 60-80%
- Other rheum labs that can be seen in Sjogren’s but nonspecific and does not help with diagnosis: ANA+, RF+
- CBC with differential: anemia of chronic disease
- RF+ (+/- low C4) independently associated with higher risk of non-Hodgkin’s lymphoma in primary Sjogren’s
- Given features can overlap with SLE, consider checking other extractable nuclear antigens
Objective Testing
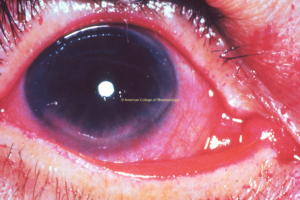
- Ocular surface staining (view image)
- Salivary gland scintigraphy
- Whole sialometry
- Salivary gland biopsy
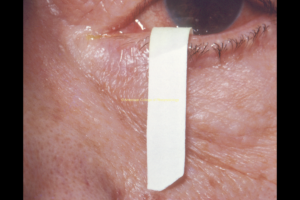
- Schirmer test (view image)
- Extraglandular evaluation driven by organ(s) involved
- Concern for interstitial lung involvement: CT ILD protocol
- For peripheral small fiber neuropathy: skin biopsy may be needed (EMG/NCV will not
pick up small fiber neuropathy)
Sicca (Dry Eyes and/or Dry Mouth)
- Age-related
- Medications:
- Anticholinergic medications
- Rheumatic diseases
- Endocrinopathy
- Diabetes
- Thyroid disease
- Infection
- Hepatitis C
- HIV and diffuse infiltrative lymphocytosis syndrome (DILS)
- Tuberculosis
- Malignancy
- Lymphoma
- Past head/neck irradiation
- Solid tumors
- Toxins
- Contact use (dry eyes/xerophthalmia)
- Smoking
Avoid contributing medications and desiccants
Oral Symptoms
- Good hydration
- Salivary stimulants
- Artificial saliva
- Muscarinic agonist: pilocarpine, cevimeline
- 1.1% sodium fluoride
- ENT referral if oral ulcers, refractory disease
Ocular Symptoms
- Artificial tears/ointment
- Ophtho referral:
- Topical cyclosporine
- Punctal plugs
Extra-Glandular Manifestations
Poor Prognostic Factors
- RF+ (+/- low C4) independently associated with higher risk of non-Hodgkin’s lymphoma in primary Sjogren’s
- Disappearance of previously positive RF concerning for development of lymphoma
- Low complements
- Parotid gland enlargement
- Lymphadenopathy
Complications
- Increased risk of non-Hodgkin’s lymphoma
- Cryoglobulinemic vasculitis
- Important to rule out mimics: oral candidiasis, medications, smoking, contacts overuse
- 25-60% of peripheral neuropathy precedes Sjogren’s diagnosis
- If sicca but SSA/SSB neg: consider cancer or IgG4 disease, recommend biopsy
- Sjogren’s can be associated with cryoglobulinemic vasculitis (consider this diagnosis if new rash; labs will show very low C4, normal C3, high RF)
- RF+, parotid gland enlargement, +/- low C4 in adults independently associated with higher
risk of non-Hodgkin’s lymphoma in primary Sjogren’s