About Juvenile Dermatomyositis
Juvenile dermatomyositis (JDM) is an inflammatory, autoimmune disease that primarily affects skin and muscles.
- Peak age of onset: 7 yo
- Range: 1-15 yo
MSK Exam
- Muscle weakness primarily in proximal limb-girdle, neck, and trunk
- Difficulty rolling over, difficulty getting up stairs; may have Gower’s sign when getting up from floor; may have problems raising head off bed while prone
- Assess presence of symmetric palatal elevation and gag reflex; if asymmetric/absent, requires emergency medical care
- Loss of milestones or delay in obtaining milestones
Skin
- Heliotrope rash (view image)
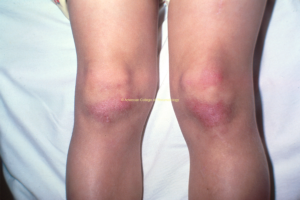
- Gottron’s papules (view images)
- Malar rash/facial erythema (view images)
- Calcinosis (view image)
Other Organ Involvement
- Respiratory (interstitial lung disease)
- GI (dysphagia, aspiration, intestinal vasculopathy)
- Cardiac (cardiomyopathy)
Lab Workup
- Muscle enzymes (typically elevated): CK, AST, ALT, LDH, aldolase
- Values may not all be elevated simultaneously.
- For patients who are very physically active in sports, in the absence of significant rash and weakness, when muscle enzymes are elevated, have patient abstain from exercise x2 weeks and repeat
- CRP and ESR may not be markedly elevated.
- If patient has had long-standing disease, lab values may be normal or near normal.
Imaging
- MRI w/o contrast to look for muscle enhancement, muscle atrophy, and/or fatty infiltration
- X-rays can show calcinosis in extremities.
Pharmacologic
- Corticosteroids (wean over time)
- Methotrexate
- IVIG
- Hydroxychloroquine (good for skin disease)
- Topical corticosteroids and topical tacrolimus for rash
Non-Pharmacologic
- Physical therapy
- Occupational therapy
- Sun protection/decreased UV exposure
- Monitor for other organ involvement (cardiac, lung, GI)
- Annual PFT
- Dexa screening for chronic steroid use
- Early treatment to prevent:
- Joint contractures
- Irreversible skin damage
- Appropriate growth of muscles and bones
- Calcifications due to poorly controlled disease
- Risk for osteopenia and pathologic fractures from steroids
- ⅓ will go into permanent remission, ⅔ will have chronic course
- Specific myositis antibodies can be obtained to help ascertain disease pattern and prognosis; also helps direct monitoring
Clinical Presentation
- Muscle weakness is a prominent symptom, not myalgia.
- Vast majority of patients with JDM have skin disease
- Dermatomyositis in children is rarely associated with malignancy (unlike adults, where this is often the case).
- Bones are often weak due to chronic inflammation and/or steroid therapy.
- Involvement of neck muscles puts patient at risk for aspiration and must be treated aggressively.
Diagnostic Workup
- Muscle biopsy is rarely needed for diagnoses but may be helpful in some cases.
Management
- Sun protection is important in preventing disease flare.