An 80 yo M with history of HLD and CAD presents to clinic with complaint of muscle pain and weakness in his shoulders.
History & Physical Exam
- He recently noticed pain in his temples (worse on L) and difficulty chewing because his jaw will become tired.
- He had one episode of transient vision loss in his L eye, but this resolved within 2-3 minutes and has not recurred. He has never had these symptoms before.
- He has had some low-grade fevers recently, but thought this was secondary to being around his grandchildren.
- He is also having difficulty lifting his arms above his head when he tries to wash his hair in the shower.
- On PE, he is unable to lift his shoulders above his head without discomfort, and he has tenderness to touch of his L temple. His vision is normal in clinic today.
- His vital signs are within normal limits.
Diagnostic Workup
Treatment & Management
- Start on high dose steroids (1 mg/kg)
- Schedule temporal artery biopsy within the next 2 weeks
- Consider start of tocilizumab to decrease steroid burden, also given patient’s CAD history
An 80 yo M with hx of HLD, CAD presents with new onset of unilateral headaches refractory to OTC medications, including NSAIDs and acetaminophen.
History
- No vision changes
- Few weeks of girdle stiffness
- Symptoms of tiredness when chewing on food for long, such as food like steak
Physical Exam
- Normal VS
- Shoulders tender to palpation bilaterally
- Scalp tender to palpation over the area of the temporal artery with diminished temporal artery pulse on right (view image)
- High-dose steroids started for high suspicion of giant cell arteritis
Diagnostic Workup
- Labs: CRP 50 mg/L, ESR >120, CBC and CMP wnl
- Biopsy:
- Temporal artery biopsy pathology obtained within 2 weeks of steroid start.
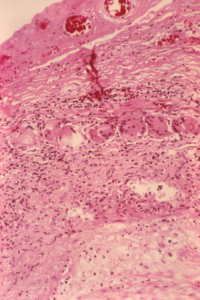
- Granulomatous inflammation of the inner half of the media, centered on the internal elastic lamina, with a mononuclear infiltrate, multinucleated giant cells, and fragmentation of the internal elastic lamina (view image)
Treatment
- High doses of systemic steroids with taper yielded improvement in headache
- Also started tocilizumab to decrease steroid burden, given patient’s CAD