About Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis (JIA) is an inflammatory autoimmune disease that primary impacts the joints.
- Group of heterogeneous disorders with the following common features:
- Onset <16 yo
- Joint inflammation in at least one joint
- Duration of at least 6 weeks
- Type of JIA determined by number of joints involved, distribution of joints involved, presence or absence of serologic markers, associated psoriasis (or psoriasis in 1st degree relative), or systemic features (fever, rash, lymphadenopathy and serositis)
- ILAR criteria remains the gold standard for defining categories of JIA but does not always dovetail with adult categorization system.
ILAR Subtypes
# and Distribution of Joints Affected
- 1-4 in 1st 6 months → persistent oligoJIA
- 4 months → extended oligoJIA
- Asymmetric
Associated Lab and Systemic Findings
- Oligo JIA with +ANA has highest risk of uveitis
Demographics
- Peak 2-4 yo
Adult Corollary
- None
# and Distribution of Joints Affected
- 4 joints
- Symmetric
- Large and small joints
Associated Lab and Systemic Findings
- +ANA has higher risk of anterior uveitis
Demographics
- Peak 2-4 yo and 6-12 yo
Adult Corollary
- Unclear; some similarity to seronegative RA
# and Distribution of Joints Affected
- 4 joints
- Symmetric
- Large and small joints
Associated Lab and Systemic Findings
Demographics
- Peak incidence in adolescence
Adult Corollary
- Seropositive RA
# and Distribution of Joints Affected
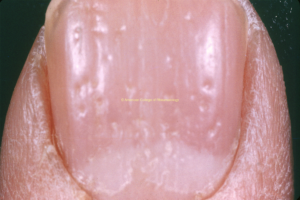
- At least one joint with arthritis AND psoriasis OR with 2 of the following: dactylitis (view image),nail pitting (view image), or 1st degree relative with psoriasis
- Small and large joints
- Often asymmetric
- Can involve axial or peripheral joints
Associated Lab and Systemic Findings
- Psoriasis
Demographics
- Peak 2-4 yo and 9-11 yo
Adult Corollary
- Psoriatic arthritis
# and Distribution of Joints Affected
- Asymmetric with axial involvement common; lower>upper extremities
Associated Lab and Systemic Findings
- HLA-B27+ more common
- Uveitis typically symptomatic
- May be seen with inflammatory bowel disease
Demographics
- Early adolescence
Adult Corollary
# and Distribution of Joints Affected
- Systemic features may greatly precede joint features
- Polyarticular>>>monoarticular
- Large and small joints
- Can involve axial or peripheral
Associated Lab and Systemic Findings
-
Elevated acute phase reactants, including ferritin
-
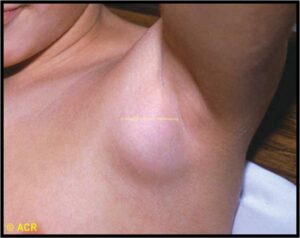
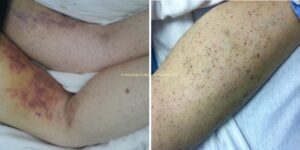
Includes quotidien fever, evanescent rash (view image), serositis, lymphadenopathy (view image)
Demographics
- Peak onset between 1-5 yo
- Equal sex distribution
Adult Corollary
- Adult onset Still’s disease
- Insidious-onset, chronic arthritis (>6 weeks) with onset ≤16 yo
- Arthritis can manifest as limitation of joint, stiffness after inactivity, swelling, or pain on motion (particularly at the extremes of range of motion).
- Pain is not required to diagnose arthritis; many children do not perceive arthritis as painful.
- Key features on history: swelling, limp, morning stiffness (that recurs after naps in toddlers), difficulty opening doors, opening bottles, self feeding, increased crying with diaper changes upon lifting pelvis, and overall inability/refusal to do activities they find enjoyable
- Joint involvement can be characterized in the following ways:
- Symmetric vs. asymmetric
- Oligoarticular (≤4 joints) or polyarticular (≥5 joints)
- Axial or peripheral
- Physical exam findings
- Acute joint inflammation: swelling, warmth, limitation of motion, pain on motion/palpation
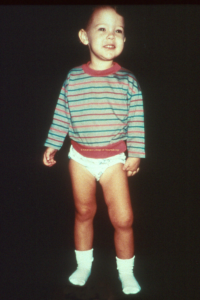
- Chronic inflammatory changes: muscle atrophy on affected side, limb length discrepancy (view image), bony overgrowth, limitation of motion, pain on motion
- Extra-articular manifestations:
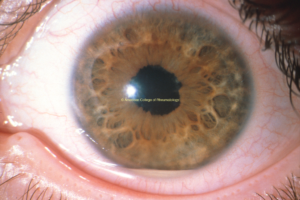
- Uveitis (view image)
- Inflammatory bowel disease
- Psoriasis (view images)
Lab workup for arthritis for ≥6 weeks
- Inflammatory markers (ESR, CRP)
- CBC for anemia of chronic disease
- Complete metabolic panel (CMP)
- Must exclude: Lyme (in endemic areas, IgG will be positive), post-streptococcal reactive arthritis, parvovirus, and other connective tissue diseases, where appropriate
- HLA-B27, rheumatoid factor, and anti-CCP antibody to help classify type of arthritis and prognosis
- ANA ONLY to help stratify risk for developing uveitis OR if SLE is in the differential diagnosis – ANA is NOT diagnostic for JIA
- Synovial fluid is rarely necessary (and is NOT required for diagnosis) unless there is inability to bear weight, significant concern for septic joint, or family history of metabolic condition causing elevated uric acid.
Imaging
- X-rays will show damage due to chronic disease but less likely to show active inflammation (caveat: knee and ankle effusions are sometimes visible).
- Musculoskeletal ultrasound, when available, can identify active inflammation.
- MRI with and without contrast will show arthritis and tenosynovitis, and will also identify anatomic/traumatic pathology.
- Contrast is helpful to show synovial inflammation.
Other Rheumatic Diseases
Including (but not limited to) the following:
- SLE
- Sjogren’s
- Sarcoidosis
- Systemic vasculitis
- SAPHO
Non-rheumatic Diseases
Including (but not limited to) the following:
- Scurvy (see image)
- Hemophilia
- Malignancy
- Acute rheumatic fever
- Farber disease (lysosomal storage disease)
Arthritis Lasting <6 Weeks
- Post-viral reactive arthritis
- Transient (toxic) synovitis
- Lyme arthritis
- Post-streptococcal reactive arthritis
- Henoch-Schonlein purpura
Treatment for Acute Inflammation
- NSAIDs: scheduled NSAIDs may decrease overall inflammation (monitor for renal or GI side effects)
- Glucocorticoids: complete evaluation prior to starting steroid
- Ideally should not be started without rheumatology involvement in new diagnosis
- High morbidity
Steroid-sparing Treatment
Minimal data from head-to-head trials, so first line choice may vary based on practitioner or may be dictated by insurance company (choice should be directed by pediatric rheumatology)
- DMARDs (methotrexate, leflunomide)
- Biologics (TNF inhibitors, IL-6 inhibitors, others)
- Ideally, follow up with rheumatologist every 3 months to identify and address occult inflammation.
- Disease activity measures utilized by specialists
- Lab monitoring every 3-6 months for medication toxicity
- Ophthalmology screening (frequency determined by type of JIA, ANA status, age at diagnosis, and time from diagnosis); AT LEAST annually by ophthalmologist to look for uveitis
- Children may not report pain associated with arthritis.
- TMJ arthritis can be involved and can be disfiguring if not treated (view image).
- Ask about pain with chewing, cracking, or difficulty with thick or wide foods.
- Uveitis can occur without symptoms but can lead to blindness.
- On exam, you can see sequelae with the ophthalmoscope by looking for irregularity in the pupillary border (view image).
- Children with Trisomy 21 can get a severe erosive polyarticular arthritis that is often difficult to treat and identified late in course.
- Having parent video child’s gait immediately upon waking and then 2 hours later may help clarify if there is morning stiffness.
- Primary treatment goal is to eliminate active joint and tendon inflammation to prevent long-term irreversible damage.