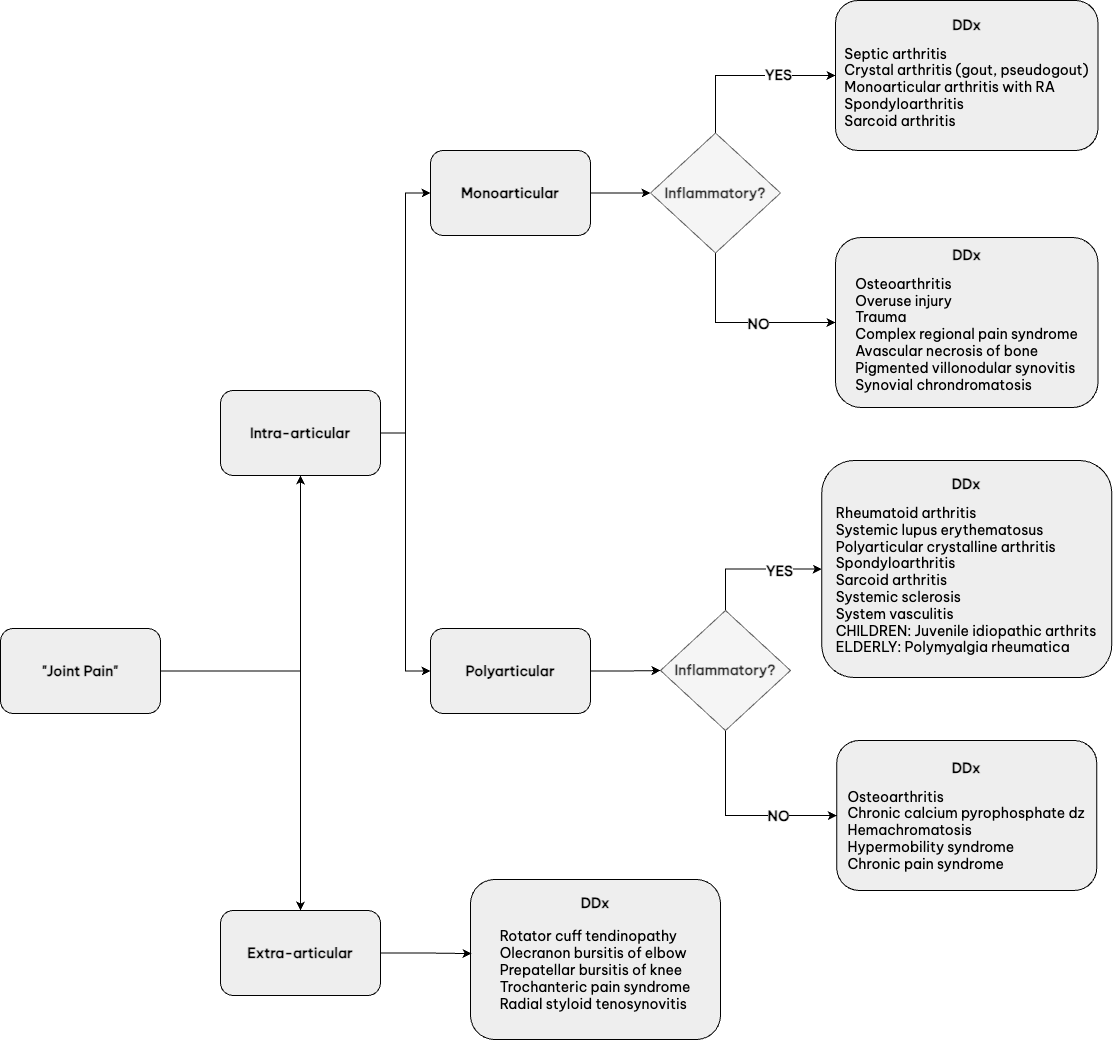
When a patient reports symptom of “joint pain,” it is very important to differentiate if the pathology is truly within the joint (intra-articular) or an issue with structures around the joint (extra-articular).
- INTRA-ARTICULAR:
- Pain on ACTIVE range of motion or when the patient does the movement, and
- Pain on PASSIVE range of motion or when the provider does the movement
- EXTRA-ARTICULAR:
- Pain on attempted ACTIVE range of motion
- Commonly painless on PASSIVE range of motion or when the provider does the movement
- Tenderness on palpation of peri-articular structure
An important factor in developing a more focused differential is to determine whether the joint problem is inflammatory versus non-inflammatory in nature:
- INFLAMMATORY:
- On history: AM stiffness usually ≥60 min, improves with activity
- On physical exam: swelling, effusion, warmth, and erythema of joint
- If joint fluid available (look for WBC amount, gram stain, culture, and crystals): WBC ≥2k (and not hemarthrosis)
- NON-INFLAMMATORY:
- On history: AM pain usually ≤ 30 min, worsens with use
- On physical exam:
- Crepitus +/- locking, clicking
- Bony hypertrophy (longstanding OA) or effusion may be present, but the joint will not be warm and soft tissue swelling will be absent.
- If joint fluid available: WBC <2K
Given the above, the following approach is recommended for diagnosing patients with joint pain.
- Chronicity
- Acute onset: crystal arthropathy (in adults), infection
- <6 weeks: parvovirus, Epstein Barr virus, Lyme, post-streptococcal reactive arthritis
- Chronic (≥6 weeks): osteoarthritis, rheumatoid arthritis, spondyloarthropathies, systemic lupus erythematosus and related connective tissue disorders, sarcoid, juvenile idiopathic arthritis (in children), polymyalgia rheumatica
- Septic arthritis
- Sexually active: gonococcal infection
- IV drug use: staph or strep septic arthritis
- Sickle cell: salmonella
- Diarrhea: consider enteropathic arthritis or reactive arthritis
- Urinary tract infection symptoms: reactive arthritis
- Anticoagulated: hemarthrosis
- Long-term steroid use: infection, avascular necrosis, fragility fracture
- Distribution
- 1st MTP arthritis: gout, “podagra”
- 5th MTP erosion: rheumatoid arthritis
- DIP arthritis +/- erosions or fluffy periostitis: Psoriatic arthritis
- CMC arthralgia: osteoarthritis
- MCPs 2/3: CPPD, hemochromatosis, rheumatoid arthritis
- Sacroiliac joint: ankylosing spondylitis, axial involvement with IBD-associated arthritis, psoriatic arthritis or reactive arthritis
- Rheumatoid arthritis does not involve:
- DIP
- Thoracolumbar spine
- Osteoarthritis does not involve:
- MCP
- Elbow
- Rarely glenohumeral shoulder joint
- Gout does not involve the axial spine.
The cause of a swollen joint or limp in a child varies from benign to serious and distinguishing characteristics can be elucidated from the history, examination, laboratory, and imaging studies.
History
- Trauma
- Duration, location, frequency, intensity, quality, exacerbating/alleviating factors
- Symptoms that may be associated with inflammatory joint pain:
- Morning stiffness, swelling, stairs, weakness, pain with chewing, number of joints involved
- Associated symptoms: rashes; fevers; oral/nasal ulcers; Raynaud’s phenomenon; eye problems such as conjunctivitis, iritis, or uveitis
- Symptoms associated with chronic pain syndromes:
- Evening pain
- Pain without swelling, or limited ranges of motion
- Missed school
- Association with poor quality of sleep
- Allodynia
- Associated symptoms: headaches, stomachaches, IBS symptoms, POTS
Physical Exam
- Limitation of motion: best appreciated at ENDPOINTS of range and compared to contralateral side; contractures can also be seen
- Warmth
- Swelling: best appreciated from midline while looking at both sides to compare
- Growth discrepancies: leg length discrepancy, muscle atrophy on affected side
- Gait with walking, running, toe walking and heel walking; assess for equal time on each side and foot/ankle positioning, knee flexion/extension
Differential Diagnosis
Inflammatory Arthralgia
- Systemic rheumatic diseases (including Kawasaki disease, chronic nonbacterial osteomyelitis/chronic recurrent multifocal osteomyelitis)
- Reactive and post-infectious arthritis (including rheumatic fever)
- Hematologic disorders (leukemia, bleeding diatheses, hemoglobinopathies)
- Septic arthritis and osteomyelitis (including parvovirus-associated arthritis and Lyme arthritis)
Non-inflammatory Arthralgia
- Avascular necrosis and epiphyseal disorders (Legg-Calve-Pertes)
- Traumatic arthritis including hypermobility associated with microtrauma
- Metabolic and endocrine disorders (including Rickets)
- Tumors
- Idiopathic pain syndromes (including complex regional pain syndrome and fibromyalgia)
- Vitamin C deficiency
Joint Pain Without Joint Swelling
- Legg-Calvé-Perthes disease (hip pain)
- Slipped upper femoral epiphysis/slipped capital femoral epiphysis (hip pain)
- Benign hypermobility syndrome
- Inherited metabolic disorders (e.g., Gaucher disease)
- Osgood-Schlatter disease
- Scheuermann disease
- Growing pains
- Complex regional pain syndrome
- Amplified musculoskeletal pain
Single Joint Involvement
- Bacterial infections (e.g., septic arthritis, osteomyelitis, abscess and pyomyositis)
- Lyme disease in endemic areas
- Trauma
- Hemarthrosis due to vascular malformation, or bleeding diathesis
- Malignancies such as acute lymphoblastic leukemia and malignant tumors
- Benign tumors such as osteoid osteoma, pigmented villonodular synovitis
Multiple Joint Involvement
- Reactive arthritis
- Viral arthritis
- Systemic lupus erythematosus
- Juvenile dermatomyositis
- Juvenile idiopathic arthritis
- IgA vasculitis (Henoch-Schönlein purpura)
- Scleroderma
- Lyme disease
- Malignancy
- Immunodeficiency-associated arthritis
- Inflammatory bowel disease-associated arthritis
- Chronic recurrent multifocal osteomyelitis