Muscle Weakness
The first step in diagnosing a patient presenting with muscle weakness is to consider the following:
- Subjective: Is it malaise (i.e. functional limitations with preserved muscle strength)? If so, unlikely that it is inflammatory myopathy.
- Objective: Is there objective weakness on physical examination?
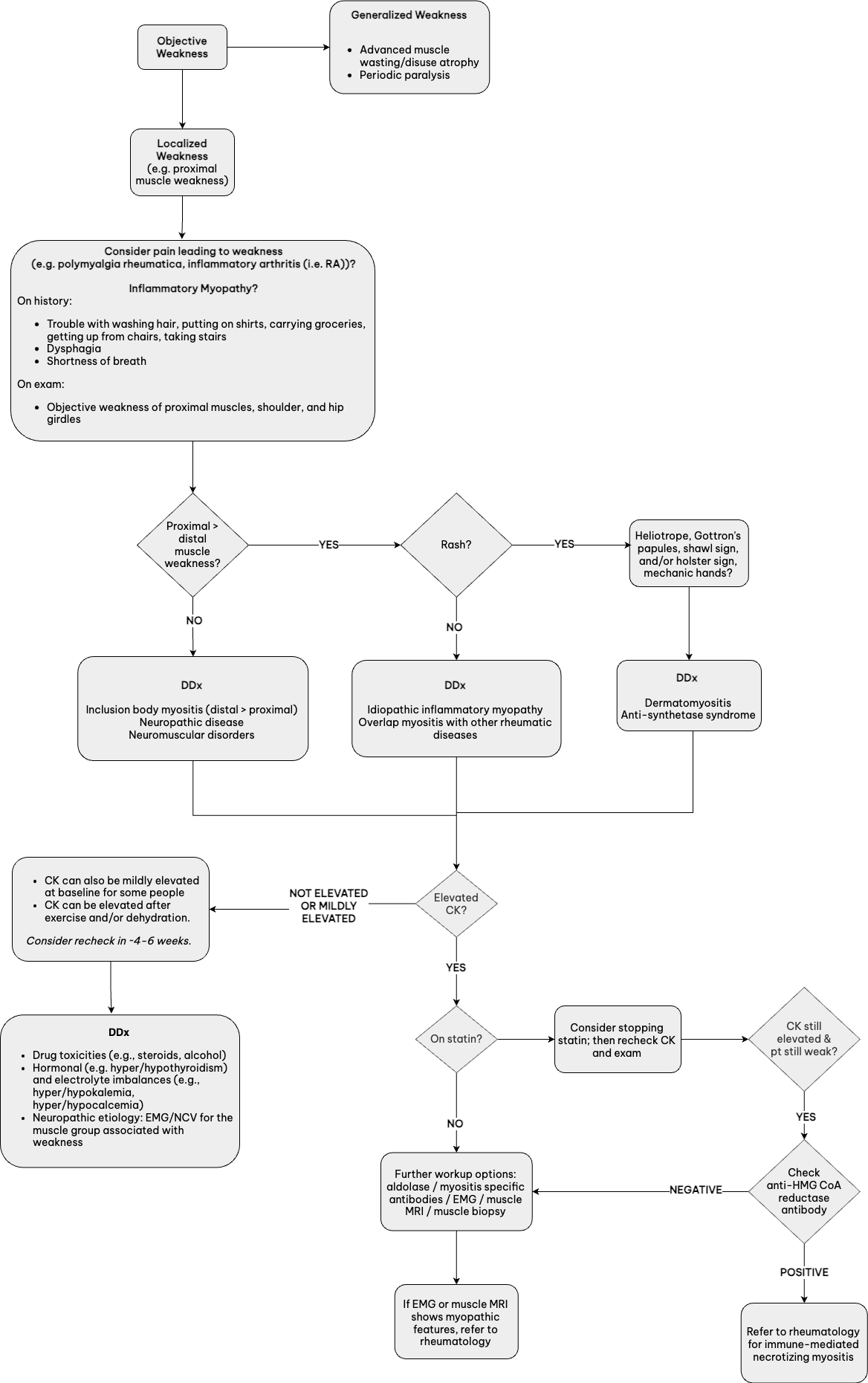
- See flowchart below for further guidance.
Inflammatory myopathy tends to have a predominance of weakness over pain. Weakness is progressive over weeks to months instead of acute onset.
Presentation
- In patients with true inflammatory myositis:
- Functional limitations are the most common presenting symptom, rather than pain.
- Muscle tenderness usually absent (exceptions: infectious myositis, metabolic myopathies, necrotizing myopathies)
- Dermatomyositis can present without muscle weakness, known as clinically amyopathic dermatomyositis (CADM), associated with autoantibody: MDA-5
- Juvenile dermatomyositis typically has more skin manifestations than muscle disease
- Immune mediated necrotizing myositis can be statin induced, but also consider substances with statin-like qualities such as red yeast rice and oyster and shiitake mushrooms
Labs
- Routine labs provide clues to diagnosis:
- Anemia on CBC can indicate anemia of chronic disease
- AST/ALT can be surrogate markers for high muscle breakdown if no CPK
- Thyroid function tests can assist in elucidating etiology
- CPK: highest sensitivity for muscle disease
- If no, CK available, it can be added onto basic or comprehensive metabolic panel and AST/ALT can be surrogate markers for high muscle breakdown.
- Not all patients with inflammatory myositis have a positive ANA
- Drug toxicities such as steroid-myopathy often presents with normal CKs
Monitoring and Screening
- Inclusion body myositis (IBM) can be misdiagnosed as polymyositis and is typically resistant to treatment.
- Myositis not responding to treatment should be evaluated for IBM.
- Many patients with myositis can have interstitial lung disease, which can be a cause of death.
- Dermatomyositis, as compared to other inflammatory myopathies, is more commonly associated with malignancy; therefore age-appropriate malignancy screening should be considered with these patients, especially with the following autoantibody positivity: TIF-1-gamma, NXP-2.
History
- Nearly all pediatric inflammatory myositis affects proximal muscles
- In young children, can see regression in walking, and difficulty rolling over and going from sitting to standing
- In older children, can see difficulty in getting up tall step (i.e., school bus), difficulty styling hair, etc.
Physical Exam
- Gottron’s papules are PATHOGNOMONIC!
- Rash on knuckles often confused for warts
- Can also occur on elbows, toes, and knees
- May have palatal erythema or ulceration (may be painless)
- May have heliotrope rash, malar rash, calcinosis – shawl sign can occur but less common than in adults
- Validated tool for assessment of proximal muscle weakness: Childhood Myositis Assessment Scale
- Pulmonary disease may be present in some patients
- Arthritis can co-occur
Labs
- CPK normal values may depend on individual muscle mass; therefore, in small, lean child, normal CPK does not exclude myositis
- Adolase, AST, and ALT may also go up in myositis
- Levels may be falsely elevated in patients with high levels of physical activity; if abnormal, may need child to avoid sports for 1-2 weeks prior to blood draw repeat
Clinical Pearls
- Dermatomyositis in children is not commonly associated with malignancy (unlike in adults)
- In absence of classic findings, rule out viral-induced myositis, or rhabdomyolisis
- Patients with dermatomyositis may have a positive ANA
Muscle Pain
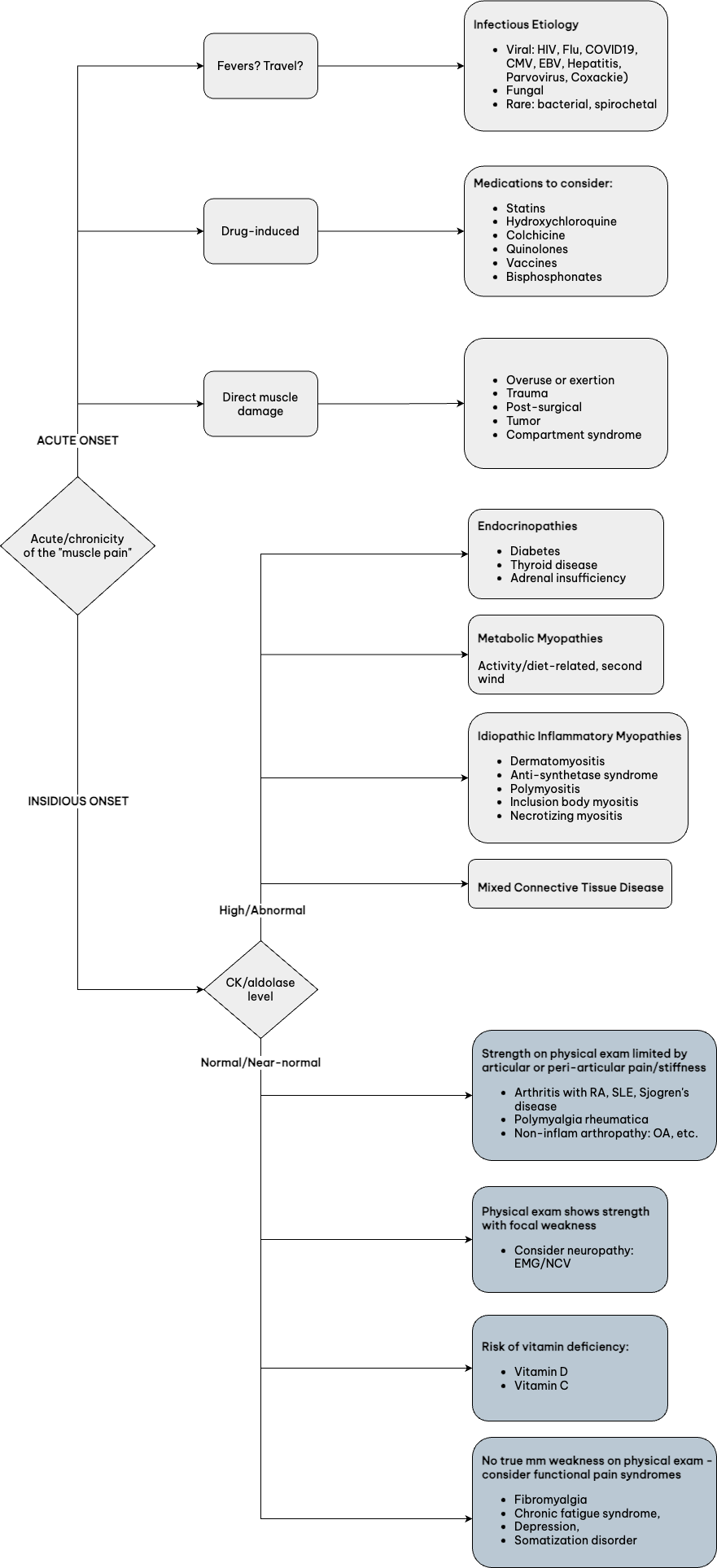
When diagnosing a patient with muscle pain, the first step is determining if the pain had an ACUTE ONSET or INSIDIOUS ONSET. View the recommended diagnostic workup for each below.
Idiopathic Inflammatory Myositis (IIM)
- Inflammatory myopathy tends to have more weakness and rarely have pain (unless necrotizing or very advanced)
- Necrotizing myopathy: consider HMG-CoA antibody (even without hx of statin tx), SRP antibody
- Rash identification is key for IIM:
- Heliotrope rash, shawl rash, holster sign, etc.: dermatomyositis
- Hand peeling: “mechanic’s hand” and anti-synthetase syndrome
Biopsy
- Localization or site of most symptoms will guide diagnostic evaluation regarding imaging and/or EMG/NCV.
- Do not biopsy:
- On the same side as EMG/NCV – will lead to nonspecific mm changes and harder to get diagnosis
- During rhabdo – will not yield clinically useful results
Rheumatic Diseases
- Rheumatoid arthritis/systemic lupus erythematosus, SJS, vasculitis: Myalgias are common with slight elevation of CKs but true myositis rare
- Mixed connective tissue disease can have CK elevated into 100s or low 1000s, alongside features of SLE/systemic sclerosis
Medications
- Keep in mind CYP P450 interactions that may increase risk of culprit medication toxicities for myopathy
Other
- Reflexes preserved in muscle pathology except when advanced