About Spondyloarthritis
Spondyloarthritis is a group of related disorders, including:
- Psoriatic arthritis
- Ankylosing spondylitis
- IBD-associated arthritis
- Reactive arthritis
Patients are typically negative for RA antibodies (RF, CCP).
Typical Manifestations
- “Inflammatory back pain”
- Age <40 yo
- Better with activity
- Worse with immobility
- Nocturnal symptoms
- Alternating buttock pain
- Other arthritis
- Predilection for knees, ankles
- Psoriatic arthritis most likely to involve hands
- Enthesitis
- Dactylitis (“sausage digit”) (view images)
- Uveitis
Association with Derm and GI Diseases
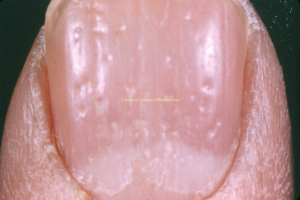
- Psoriatic arthritis: look for nail pitting (view image)
- Gut disease:
- Crohn’s disease
- Ulcerative colitis
- Infection (reactive)
- Usually GU/GI infection
Lab Workup
Synovial Fluid
- Inflammatory (2K-50K WBC/microL)
Imaging
- Sacroiliac* joints
- X-ray (view image)
- MRI with STIR: Sclerosis, erosions, “pseudo-widening,” fusion if advanced
- Peripheral joints
- Can show “pencil-in-cup” deformity for hand (view image)
- +/- extra bone formation at entheses: nonspecific
* Axial spondyloarthritis can be radiographic (patient with symptoms of inflammatory pain of back and/or sacroiliac joints WITH signs of structural change on spinal x-ray) versus non-radiographic (patient with symptoms of inflammatory pain of back and/or sacroiliac joints WITHOUT signs of structural change on spinal x-ray)
Other Rheumatic Diseases
Infectious
- Gonococcal arthritis
- Infectious sacroiliitis (typically unilateral)
Non-Inflammatory
- Osteoarthritis
- Mechanical back pain/degenerative disease
- Fibromyalgia
- Diffuse idiopathic skeletal hyperostosis (DISH)
Peripheral Arthritis
- NSAIDs
- Oral agents:
- Sulfasalazine
- Methotrexate
- Apremilast, PO – for psoriatic arthritis
- JAK inhibitors
- Biologics:
- TNF-alpha inhibitors
- Adalimumab SQ
- Certolizumab pegol SQ
- Etanercept SQ (do not use for uveitis or IBD)
- Golimumab, SQ or IV
- Infliximab IV
- IL12 and/or IL23 inhibitors:
- IL17 inhibitors
- TNF-alpha inhibitors
Note that IL17 inhibitors can exacerbate inflammatory bowel disease and should be avoided in such patients.
Axial Arthritis
- NSAIDs first line
- TNF inhibitors
- IL-17 inhibitors
- JAK inhibitors
General Measures
- Treat infection if reactive arthritis
- Physical therapy
- Coordinate with dermatology or GI
Monitoring
- Monitoring for complications of therapy
- Reactive arthritis
- Many cases resolve (months), but minority develop chronic arthritis requiring ongoing treatment
Complications/Associations
- Inflammatory eye disease – uveitis, conjunctivitis
- Ankylosing spondylitis
- Aortic regurgitation
- Aortitis
- Apical pulmonary disease
Disease Overview & Clinical Presentation
- Inflammatory arthritis of DIPs – PsA high on DDx
- Inflammatory back pain of young
- Start with SI joint radiographs
- Classic triad of reactive arthritis = conjunctivitis, urethritis, and arthritis
- Most patients do NOT have all three features
Diagnostic Workup & Differential Diagnosis
- High suspicion for sacroiliitis
- Negative XR, consider STIR MRI of pelvis
- HLA-B27 positive has high population prevalence
- HLA-B27+ doesn’t equate to spondyloarthritis diagnosis
- If suspicious for psoriatic arthritis but don’t see obvious psoriasis, examine ears, scalp, umbilicus, gluteal cleft
- Spinal fusion in ankylosing spondylitis associated with increased risk of spinal fracture
Treatment
- NSAIDs first line for spondyloarthritis