A 33 yo M with no significant past medical history presents to the primary care clinic with low back pain.
Questions to Ask
- Inflammatory back pain that is worse in the morning or with inactivity, and better with use or activity?
- Duration of symptoms?
- Other joint complaints?
- Other organ systems involved (e.g., eyes, skin, bowels)?
- Prior treatments?
Clinical Presentation & History
- Initially developed low back pain and stiffness several years ago
- Previously responded well to occasional ibuprofen, but now having breakthrough symptoms despite scheduled use 3x per day
- Symptoms worst in morning, begin to improve somewhat after 2-3 hrs, but re-worsen with inactivity
- Also notes heel pain and swelling over the last few weeks (view image)
Diagnostic Workup
History suspicious for ankylosing spondylitis
Recommended Labs & Imaging
- Labs:
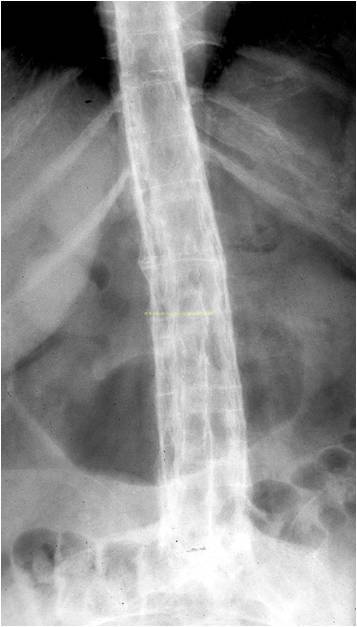
- Imaging: SI joint radiographs and heel X-ray
Test Results
- SI joint radiographs show bilateral sclerosis and erosions consistent with sacroiliitis (view image)
- Labs show CRP 1.5x ULN and +HLA-B27
Referral
Refer to rheumatology
Treatment & Further Workup
- If no contraindications, start on full dose NSAID (e.g., naproxen 500 mg BID, meloxicam 15 mg daily, ibuprofen 800 mg TID)
- If not improving after 2-4 wks, consider trial of alternate NSAID
- Second line therapies include: TNF-inhibitor, IL-17 inhibitor, JAK inhibitor, etc.
- Evaluate for other subspecialty needs:
- Bowel disease
- Uveitis
- Psoriasis
A 25 yo M with no significant past medical history presents to the primary care clinic with knee joint pain and swelling, rash, and dysuria + new penile discharge.
Questions to Ask
- Inflammatory back pain that is worse in the morning or with inactivity, and better with use or activity?
- Duration of symptoms?
- Other joint complaints?
- Other organ systems involved (e.g., eyes, skin, bowels)?
- Prior treatments?
Clinical Presentation & History
- New pain in both knees and ankles x2 weeks
- Worse in the mornings
- Improved with activity
- Physical exam:
- Right knee effusion (view image)
- Hyperkeratotic rash on palms and soles (view image)
- ROS
- Dysuria
- Penile discharge a few weeks ago after new sexual partner
Diagnostic Workup
Labs & Imaging
- Labs: CBC with diff, CMP, ESR, urine chlamydia, gonorrhea, +/- other STIs
- Imaging: plain radiographs of symptomatic joints
Test Results
- Blood tests unremarkable
- Knee x-ray:
- Effusion
- Soft tissue swelling
- Otherwise normal
- Urine PCR:
- +Chlamydia
- -Gonorrhea
- Synovial fluid:
- 18K WBCs/mm3 (58% PMNs)
- Negative crystals/Gram stain/culture
Treatment
- Treat chlamydia infection
- If no contraindications, start on full dose NSAID (e.g., naproxen 500 mg BID, meloxicam 15 mg daily, ibuprofen 800 mg TID)
- Second-line treatments include steroids (systemic or intra-articular), sulfasalazine, etc.
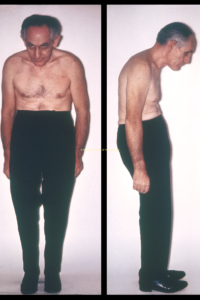
A 72 yo M with stooped posture (view image) presents to the clinic with breathing difficulties. He has not sought healthcare for many years.
Questions to Ask
- Duration of symptoms?
- Associated symptoms (e.g., cough, fever, orthopnea)?
- Musculoskeletal complaints?
History & Physical Exam
- ROS
- Dyspnea and orthopnea worsening x several weeks
- Swelling in both legs
- Physical exam
- Rales at bilateral lung bases
- Diastolic murmur
- Chronic back pain starting in late 20s
Diagnostic Workup
Labs & Imaging
- Basic bloodwork: CBC with diff, CMP
- Dyspnea evaluation: EKG, CXR, TTE, etc.
- Imaging: x-ray of his spine for stooped posture
Test Results
- Evaluation shows acute decompensated heart failure, with TTE showing severe aortic regurgitation → valve surgery
- Spinal X-ray: fusion of his SI joints bilaterally (view image), as well as thin bridging syndesmophytes throughout his spine (view image)
Referral
- Refer to rheumatology
Management
- Patient with known ankylosing spondylitis should be monitored for this complication and referred as necessary in order to prevent advanced disease and decompensation.
Clinical Pearl
- Aortic regurgitation and aortic root disease are rare late complications of ankylosing spondylitis.