About Sarcoidosis
Sarcoidosis is an autoimmune disease with increased inflammation and organ infiltration driven by granuloma formation.
- Average age of diagnosis: 40-55 yo
- Risk factors:
- Family history (strongest)
- Human leukocyte antigens (HLA) association
- Environmental: inorganic and organic materials (dust, mold, silica, metals, etc.)
Classic Presentations
May not need bx for confirmation
- Lofgren: arthritis (ankles, knees), erythema nodosum, bilateral hilar lymphadenopathy
- Heerfordt: parotiditis, uveitis, fevers, +/- facial nerve palsy
Organ Related
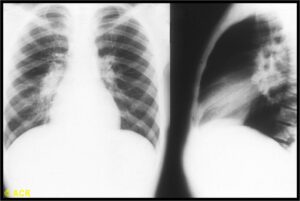
Pulmonology
- 90-95% pulmonary involvement
- Hilar LN (view image)
- Endobronchial
- Interstitial lung disease
- pHTN
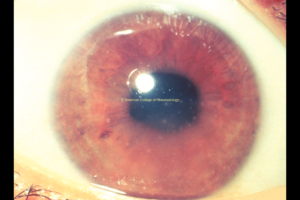
Ophthalmology
- Anterior uveitis-most common (view image)
- Can cause anterior, intermediate, and/or posterior uveitis or panuveitis
- Lacrimal gland swelling
Dermatology
- Erythema nodosum is a panniculitis
- Lupus pernio (see image) is a pathognomonic for sarcoidosis
- Non-caseating granulomatous skin lesions
- May present as raised lesions in tattoos (see image)
Cardiac
- Arrhythmia and conduction abnormality
- Infiltrative cardiomyopathy
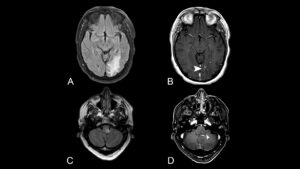
Neurology
- CN palsy
- Sensorimotor polyneuropathy (view image)
- Leptomeningeal involvement
MSK
- Polyarthritis
- Osseous involvement (view image)
Lab Workup
- CBC, CMP, ESR, CRP
- Watch for hypercalcemia
- Serum angiotensin-converting enzyme (ACE)
- Poor specificity and sensitivity!
- Supportive, not diagnostic
- Vitamin D 25-OH, vitamin D 1,25-OH
- High conversion of vitamin D 25-OH to vitamin D 1,25-OH contributes to hypercalcemia in sarcoidosis
Imaging
- High-resolution chest CT: more sensitive than CXR
- Suspected cardiac sarcoid: need cardiac MRI or cardiac PET
Tests
- Baseline PFTs
- Baseline ophthalmology exam
- Baseline EKG
Histology
- Shows well-circumscribed, compact, non-caseating granulomas of the epithelioid type rimmed by hyaline collagen
- If necrotizing/caseating features on histopathology, consider alternate diagnosis,
although can be seen in sarcoidosis
- If necrotizing/caseating features on histopathology, consider alternate diagnosis,
- Erythema nodosum histopathology will show panniculitis
Infections
- Mycobacterial
- Fungal
- Mycoplasma
- Pneumocystis jiroveci pneumonia (PJP)
- Brucellosis
- Toxoplasmosis
Environmental
- Berylliosis
- Tattoos
- Hypersensitivity pneumonitis
- Inorganic agents
Drug Induced
Other Autoimmune Disease
- Small-vessel vasculitis
- Inflammatory bowel disease
- Behcet’s syndrome
- Rheumatoid nodules
Other
- Cancer
- Lymphocytic
- Interstitial pneumonia
Who needs immunosuppression?
- Not all patients!
- Symptomatic (baseline or exertional)
and/or - Significant abnormalities on imaging or PFTs:
- Severe reticular disease
- Traction bronchiectasis
- Mod-sev low FVC or DLCO
- Symptomatic extra pulmonary manifestations
Initial Therapy
- Steroids (prednisone 20-30 mg/d, 6 mo taper)
- Consider:
- Organ involved
- Disease severity
- Comorbidities
Second-line Therapy
Includes but is not limited to:
- Methotrexate
- Leflunomide
- Mycophenolate
- Azathioprine
- TNFi like infliximab
Monitoring
- Labs: CBC and differential, creatinine, calcium, LFTs, 25 hydroxy and 1,25 dihydroxy vitamin D at least every year
- Repeat ophthalmologic exams annually or with development of symptoms: ocular pain, scleral redness, vision changes
- EKG at least every year, and monitor for symptoms of cardiac involvement – new arrhythmia, new heart failure – to see if more frequent cardiac evaluation needed
- Any new symptom of pulmonary involvement; consider spirometry every 3-6 mos with consideration of chest imaging
- Many do not ever develop symptoms and hence don’t ever require therapy.
Prognosis
- After treatment, many patients have spontaneous remission
- Other patients have chronic active disease
- Lofgren’s syndrome prognosis good!
- 70-80% of patients in remission 2 yrs after diagnosis
- Classic presentations (Lofgren’s, Heerfordt) most times do not need histology for diagnosis and steroid can be started without biopsy.
- 90-95% patients have pulmonary involvement.
- Most common: hilar lymphadenopathy (view image)
- Upon diagnosis of sarcoidosis, even without ocular symptoms, need baseline EKG and ophthalmologic exam
- Ruling out infection is critical as immunosuppression is the cornerstone for sarcoid therapy
- Not all patients need immunosuppressive therapy!