About Henoch-Schönlein Purpura
Henoch-Schönlein purpura (HSP) is one of most common types of vasculitis in children.
- Rarely may occur in adults
- Most common in children ages 3-15 yo
- M > F (1.5:1)
- Pathogenesis unknown
- Possible infectious triggers include streptococcal infection and viral illness
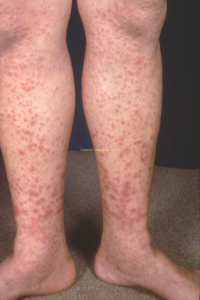
Skin – Palpable Purpura (100%)
- Dependent surfaces (legs/buttocks) more affected (view image)
- Small petechiae to large ecchymoses, rare bullae/ulcerations
- SQ edema (hands, feet, eyes, scrotal) (view image)
GI (~66%)
- Colicky pain
- Blood in stool
- Intussusception
- Symptoms may precede skin manifestations by up to a week
Renal (~33%)
- Range: mild blood/protein – nephritic/nephrotic syndrome/renal failure
- Hypertension
MSK (50-80%)
- Large joints (knees, ankles) > smaller (wrists, elbows, fingers)
Other (Rare)
- CNS, lung, ocular
- Fever is rare but may occur as part of prodrome
Lab Workup*
- CBC (rule out thrombocytopenia)
- CMP (renal function)
- Urinalysis (hematuria/proteinuria)
- Stool guiac if having significant GI symptoms
- ESR/CRP may be normal or elevated.
*If other vasculitides are being considered based on presentation, additional testing should be guided by clinical suspicion.
Pathology
- Skin:
- Leukocytoclastic vasculitis (granulocytes in arteriole/venule walls)
- IgA deposits
- Renal:
- Endocapillary proliferative glomerulonephritis (GN)
- IgA on IF
Imaging
- Abdomen U/S if concern for intussusception
- Systemic lupus erythematosus
- Other vasculitis (ANCA-associated, polyarteritis nodosa, etc.)
- Post-strep glomerulonepthritis
- Immune thrombocytopenic purpura
- Hemolytic uremic syndrome
- Disseminated intravascular coagulation
- Sepsis
Supportive
- Hydration
- Pain control
- Tylenol PRN
- In absence of renal disease, NSAIDS for arthralgia
- Antihypertensives
Corticosteroids
- Consider for arthritis that does not respond to NSAIDs, or if NSAIDs are contraindicated
- Consider for severe abdominal symptoms
- Dosing:
- 1 mg/kg with max of 60 mg
- Taper over 2-4 weeks, as patients are susceptible to significant rebound during course.
- For significant renal disease
- Prophylactic steroids do NOT seem to prevent complications
Severe Disease
Rapidly progressive GN, pulm hemorrhage, etc., may warrant more aggressive immunosuppression.
Anticipatory Guidance
- Rash often waxes and wanes for 6 weeks but may last as long as 3 months
- Urinalysis and BP check once a week for first 6 weeks, then monthly for first 6 months of disease course; return precautions for severe abdominal symptoms
- 2/3 of children with resolution within 4 weeks
- 1/3-1/2 may have recurrence within 6 weeks or up to 2 years after onset
- Renal disease:
Disease Overview & Clinical Presentation
- Palpable purpura (view image) is often first manifestation, but sometimes preceded by GI/MSK/renal symptoms
- Disease may be driven by dysregulation of IgA-mediated immune response to antigen.
Diagnostic Workup
- Persistent intussusception may require air or contrast enema, rarely surgical intervention.
- Skin biopsy may help to confirm diagnosis if unclear.
- Renal biopsy only indicated with severe nephritic/nephrotic syndrome, impaired renal function
Monitoring and Progress
- Recurrence may occur spontaneously or be triggered by infection.
- Most children improve with supportive care only.
- Evidence is mixed regarding the benefit of steroids.