Review the following visual approach to rashes in systemic rheumatic diseases.
Important Note: Always rule out potential infectious or drug etiologies before assuming the rash is systemic in origin.
Rashes occur in parallel with other organ disease activity in systemic lupus erythematosus
Clinical Description
Flat or raised pink/red scaly rash over the cheeks and nasal bridge – “butterfly”/malar rash; can also be generalized
- Spares nasolabial folds
- Non-scarring
- Rash in between the knuckles
Brief Histopathologic Description
- Interface dermatitis with disrupted dermo-epidermal junction
Differential Diagnosis
- Rosacea: presence of red papules and telangiectasia; triggered by spicy foods
- Seborrheic dermatitis: pink-red, scaly and not itchy rash involving primarily the scalp
- Dermatomyositis: does not spare nasolabial folds; rash overlies the knuckles
- Cutaneous lymphoma
Recommended Workup
Clinical Description
- Well demarcated coin shaped, red, and scaly papules or plaques in sun–exposed areas
- Result in atrophic (central) scarring and dyspigmentation (borders)
Brief Histopathologic Description
- Interface dermatitis with disrupted dermo-epidermal junction
Differential Diagnosis
- Discoid lupus: 28 % with generalized rash can develop SLE
- Discoid mimics:
- Actinic keratosis
- Cutaneous tuberculosis
- Subcutaneous sarcoidosis
Recommended Workup
- ANA
- Skin biopsy may be required.

Clinical Description
- Annular polycyclic plaques with a raised red scaly border and central clearing
- Can lead to post-inflammatory dyspigmentation
- Non-scarring
- Distribution usually photosensitive areas – shoulders, arms, upper torso, upper back
Brief Histopathologic Description
- Interface dermatitis with disrupted dermo-epidermal junction
Differential Diagnosis
- SCLE occurs in 10-15% with SLE; 50% of SCLE progresses to SLE
- Drug associations include but not limited to: tamoxifen, lansoprazole, statins, ACEi, TNFi, anti-epileptics, PPIs, naproxen, etc.
- Tinea corporis
- Erythema annulare centrifugum
- Psoriasis
- Lichen planus
- Eczema
Recommend Workup


- Heliotrope, facial rash, and Gottron’s papules
- Gottron sign asymmetrical violaceous macules can also be observed
Clinical Description
- Flat violaceous scaly rash on the face
- Involves nasolabial folds and eyelids
- Symmetrical erythematosus papular lesions over the metacarpophalangeal and interphalangeal joints
- Periungueal erythema
Brief Histopathologic Description
- Interface dermatitis – unable to differentiate from skin histopathology of lupus
Differential Diagnosis
- Systemic lupus erythematosus: apares nasolabial folds and eyelids
A skin biopsy cannot help distinguish between SLE and DM.
Recommended Workup
- Creatinine kinase and aldolase levels, ANA, myositis panel
- Classic presentation may not need a skin biopsy.
- Screen for an underlying malignancy!
Clinical Description
- Limited or diffuse skin thickening and tightness (face, torso, extremities, finger “sclerodactyly“)
- Coexistence of hyperpigmentation and hypopigmentation (“salt-pepper lesions”)
- Lesions sparing the perifollicular area
- Telangiectasias on the cheeks, nose, and lips
Brief Histopathologic Description
- Thickened collagen in the dermis and dermal fibrosis
Differential Diagnosis
- Scleroderma mimics (scleromyxedema, scleredema, eosinophilic fascitis)
- No Raynaud’s phenomenon
- No sclerodactyly
- No nailfold abnormalities
- Negative serology
- Face rarely affected
Recommended Workup
- Autoantibody profile (Scl-70 [or anti-topoisomerase I], anti-centromere, RNA polymerase III)
- Screen for lung or cardiac involvement

Clinical Description
- Salmon colored edematous plaques or salmon colored edematous rash
- Evanescent rash coinciding with fever spikes
- Non-pruriginous
Brief Histopathologic Description
- Neutrophilic inflammation in the dermis
Differential Diagnosis
- Urticaria: pruriginous transient lesions
- Urticarial vasculitis:
- Hives usually persist for longer than 48 hours.
- Can be associated with low complement levels
Recommended Workup
- C-reactive protein, sedimentation rate, ferritin levels
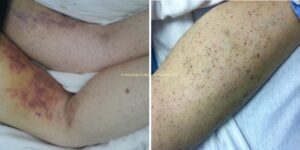
Many conditions can be associated with finding of LCV on histopathology.
- Different infections including but not limited to: streptococcal upper respiratory tract infection, mycobacterium, staphylococcus aureus, chlamydia, neisseria, and HIV, hepatitis B, hepatitis C, and syphilis.
- Systemic diseases including: any small vessel vasculitis, ANCA-associated vasculitis, cryoglobulinemic vasculitis, various connective tissue diseases, erythema elevatum diutinum
- Malignancies including but not limited to: lymphomas, leukemias, lung cancer
- Various drug associations including but not limited to: beta-lactams, erythromycin, clindamycin, vancomycin, sulfonamides, furosemide, allopurinol, NSAIDs, amiodarone, gold, thiazides, phenytoin, beta-blockers, TNF-alpha inhibitors, selective serotonin reuptake inhibitors, metformin, warfarin, valproic acid
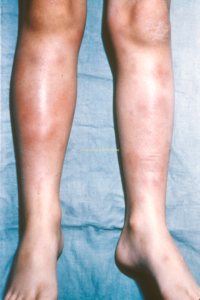
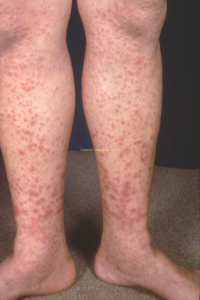
Clinical Description
- Clusters of small and large red-purple non-blanchable discoloration in the lower extremities
Brief Histopathologic Description
- Neutrophilic inflammation around the blood vessels leads to vessel wall inflammation. This causes vascular injury and extravasation of red blood cells into the dermis, hence the purpuric appearance.
Differential Diagnosis
- Leukocytoclastic vasculitis: petechia and palpable purpura (dependent areas)
- Small vessel vasculitis
- ANCA-associated vasculitis
- Cryoglobulinemic vasculitis
- Associated with connective tissue diseases
- Urticarial vasculitis syndrome
- Hypersensitivity vasculitis
- Scurvy (view images)
- Meningococcemia
- IgA vasculitis (Henoch-Schonlein purpura) (view image)
- Disseminated intravascular coagulation
- Thrombotic thrombocytopenic purpura
- Emboli: cardiac myxoma, cholesterol emboli, septic and infectious emboli
- Pigmented purpuric dermatosis
- Schamberg disease
- Gardener Diamond syndrome
Recommended Workup
Associated Systemic Conditions
Of the rheumatic diseases, sarcoidosis and Behcet’s are the most commonly associated
- Sarcoidosis
- Behcet’s syndrome
- Inflammatory bowel disease
- Strep-related illness
- TB
Clinical Description
- Several tender red subcutaneous nodules on the legs
Brief Histopathologic Description
- Inflammation in the subcutaneous fat (“septal panniculitis”) with giant cells
Differential Diagnosis
- In contrast to lupus panniculitis (lobular), E. nodosum does not cause scarring or involve the face
- Eosinophilic fasciitis
- Insect bites
Recommended Workup
- ANA, extractable nuclear antigens, rheumatoid factor, vitamin D 1,25, angiotensin converting enzyme level
- Chest x-ray
- Pathergy test, if history of recurrent oral or genital ulcerations