About IgG4-Related Disease (IgG4-RD)
IgG4-related disease (IgG4-RD) is a systemic immune-mediated fibroinflammatory disease with protean manifestations. It is almost always chronic and slowly progressive.
- Single organ involvement or multi-organ involvement
- Evidence of tumefactive and/or inflammatory lesions in an organ is necessary to establish a diagnosis of IgG4. Manifestations can include:
- Pancreatitis, pancreatic insufficiency
- Salivary and lacrimal gland enlargement and/or sicca symptoms (xerostomia, xerophthalmia)
- Lymphadenopathy
- Aortitis
- Retroperitoneal fibrosis
- Tubulointerstitial nephritis
- Pleuroparenchymal lung disease
- Pachymeningitis
- Orbital inflammation
- Thyroid disease
- Sclerosing cholangitis
- Constitutional symptoms may accompany the presence of specific organ involvement.
Lab Workup
- Can be helpful to evaluate for organ involvement, associated organ damage, and prognostic markers
- Elevated serum IgG4 concentration supports a diagnosis of IgG4-RD, but is neither sensitive nor specific for the diagnosis; up to 30% of patients have a normal serum IgG4 concentration.
- An elevated lipase (pancreatic disease), bilirubin (pancreatobiliary disease), or creatinine (renal disease) may point to specific manifestations; low C3 or C4 may suggest renal disease but is not specific.
- Low fecal elastase, micronutrient deficiencies (e.g., vitamin D or Zinc), and elevated A1c may suggest pancreatic insufficiency
- Additional testing is guided by the differential diagnosis and may include ANA and associated autoantibodies (e.g., SSA, SSB, dsDNA), ANCA, TB testing, HIV
- Serum protein electrophoresis (SPEP)
- IgG subclasses
- IgE
Imaging
- Cross-sectional imaging of the chest, abdomen, and pelvis is typically performed to screen for organ involvement (e.g., pancreatitis, retroperitoneal fibrosis)
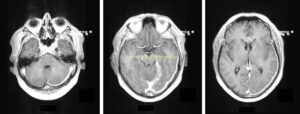
- Imaging of the head/neck may be considered if there are signs/symptoms suggestive of manifestations in the cranium (e.g., hypertrophic pachymeningitis), orbit, or salivary glands (view images)
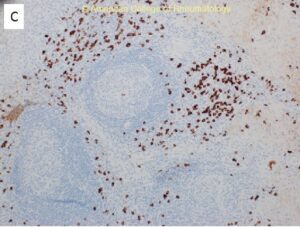
Biopsy is key! (view image)
- Biopsy may not be feasible depending on the location, and a small biopsy may not reveal all features but can be helpful to rule out malignancy and other mimicking conditions.
- An infiltrate of IgG4+ plasma cell (measured by cells per high powered field and proportion of all plasma cells) supports the diagnosis but is not specific.
- Typical histopathologic findings: lymphoplasmocellular inflammation, storiform fibrosis, obliterative phlebitis; atypical features that suggest an alternative diagnosis include necrosis, vasculitis, prominent neutrophil or histiocytic infiltrates
- Lymph node histopathology and immunostaining is not typically specific for the diagnosis of IgG4-RD.
- Malignancy should be ruled out in the case of a solitary mass (e.g., pancreatic mass, dominant salivary gland enlargement/nodule, lung mass)
- Sjogren’s disease, sarcoidosis, inflammatory bowel disease, ANCA-associated vasculitis, and other conditions can also cause salivary gland enlargement and other similar manifestations
- Primary sclerosing cholangitis is not steroid-responsive and can be distinguished from IgG4-related cholangitis.
- Castleman disease
- ANCA-associated vasculitis, Takyasu arteritis, Behcet’s syndrome
- Sarcoidosis
- Infection: fungal (histoplasmosis, etc.), viral (HIV), bacterial (TB, etc.)
- Very sensitive to corticosteroids but often relapse during steroid taper or after discontinuation!
- Rituximab can be quite effective.
- Other immunosuppressives (methotrexate, azathioprine, mycophenolate) can also be used.
- Management may also include biliary or ureteral stenting, pancreatic enzyme replacement therapy, surgical debulking for highly fibrotic lesions, and other organ-specific interventions.
- Early treatment helps prevent additional organ damage.
- Consider osteoporosis treatment/prophylaxis for those on long-term systemic steroids.
- For people with endocrine or exocrine pancreatic insufficiency, insulin, enzyme replacement therapy, and other interventions may be necessary.
- Following imaging is often used, based on manifestations, to monitor response to treatment and to assess for recurrence.
- Labs (even serum IgG4) have limited utility.
- Clinicopathologic correlation is key, and biopsy, when possible, can be useful for establishing the diagnosis and excluding mimicking conditions.
- Generally very steroid responsive – consider other diagnoses if not responding to steroids
- Disease relapses are common.
- New disease manifestations can occur over time.
- Rituximab can help considerably.