About Systemic Lupus Erythematosus
System lupus erythematosus (SLE) is a chronic, multisystem autoimmune disease.
- Autoantibodies form complexes with complement and deposit within tissues
- Multifactorial etiology: interplay between genetic, environmental, and hormonal factors
- Predominantly affects women in childbearing years but can occur in older adults and men
- Peak age of onset: 15-45 yo
- Racial and gender disparities exist in terms of organ involvement, disease severity, and response to therapy
- Reported worldwide prevalence frequencies range from 20 to 240 per 100,000 people
- Reported worldwide incidence rates range from 1 to 10 per 100,000 person-years
Heterogeneous disease
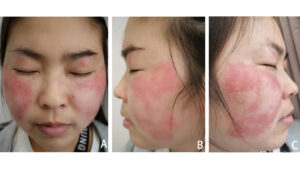
Cutaneous
(view images)- Alopecia
- Photosensitive rashes, including malar rash
- Discoid rash
Musculoskeletal
- Arthritis, especially of hands, wrists, and knees, with morning stiffness
- Jaccoud’s arthropathy (view image)
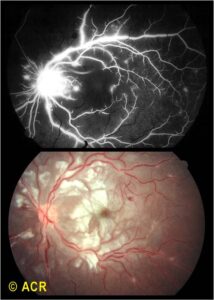
Ocular
- Periorbital swelling
- Retinal vasculitis (view images)
- Optic neuritis and other inflammatory eye conditions
Serositis
- Pericarditis and pericardial effusions
- Pleuritis and pleural effusions
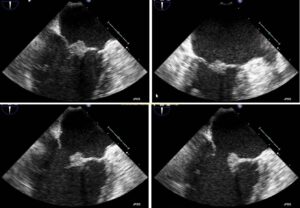
Cardiovascular
- Libman-Sacks endocarditis (view images)
- Myocarditis
- Pulmonary hypertension
Renal
- Nephritis
Hematologic
- Leukopenia
- Anemia
- Thrombocytopenia
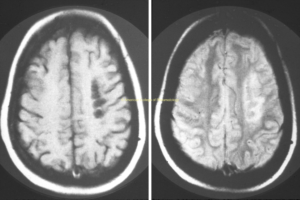
Neurologic
- Seizures
- Psychosis
- Cerebrovascular accidents (view images)
- Transverse myelitis
SLE is diagnosed clinically using a combination of clinical features and supporting labs. SLE is a very heterogeneous disease; different patients will have different manifestations.
Lab Workup
- Antinuclear antibodies (ANA)
- Laboratory hallmark of SLE
- >98% of SLE patients have a positive ANA. However, ANA is not specific for SLE (up to 33% of healthy adult population has a +ANA, but a very small percentage will develop SLE).
- Other antibodies: anti-dsDNA, anti-Smith, SSA (anti-Ro), SSB (anti-La), anti-RNP, antiphospholipid antibodies
- CBC with differential, CMP, urinalysis, urine protein: creatinine ratio, complement levels
Imaging & Biopsy
- Imaging studies and renal biopsy may be required to evaluate for certain clinical manifestations (e.g. CXR for pleural effusion, kidney biopsy for renal involvement)
Differential diagnosis is broad.
- Other connective tissue diseases:
- Scleroderma
- Sjogren’s
- Mixed connective tissue disease
- Undifferentiated connective tissue disease
- Systemic vasculitis
- Sarcoidosis
- Lymphoma
- Infective endocarditis
- Viral infections (EBV, hepatitis C, HIV, etc.)
- Sepsis
Sun Avoidance
- UV light exposure can exacerbate cutaneous rashes and cause flares.
- Patients should wear protective clothing, use sunscreen regularly, and minimize sun exposure during peak UV hours.
Pharmacotherapy
- Pharmacotherapy choice is based on organ involvement, although all patients should be initiated on hydroxychloroquine.
- The most severe organ manifestation (e.g. CNS or kidney involvement) will often dictate treatment.
General SLE Meds
- Anifrolumab
- Azathioprine
- Belimumab
- Cyclophosphamide
- Typically reserved for severe manifestations, such as CNS or kidney
- Hydroxychloroquine:
- Staple of lupus treatment
- Shown to modify disease progression in SLE and to prevent flares
- Recommended for all patients with systemic lupus
- Methotrexate
- Mycophenolate
- Local or systemic glucocorticoids for acute exacerbations
Lupus Nephritis Therapies
- Systemic steroids
- Azathioprine, PO
- Belimumab
- Cyclophosphamide
- Mycophenolate, PO BID
- Calcineurin inhibitors:
- Tacrolimus
- Voclosporin
- Disease activity measures:
- Goal is remission or low lupus disease activity
- Encourage regular clinical and lab monitoring by a rheumatologist
- Routine labs include CBC with differential, C3/C4, dsDNA, Cr, urinalysis with microscopic urine protein:creatinine
- Lupus is an independent risk factor for cardiovascular disease.
- Emphasize smoking cessation
- Manage BP, lipids using diabetes thresholds
- Screen for diabetes
- Encourage maintenance of healthy weight
- Slightly higher risk of overall cancer development
- Emphasize need for malignancy screening, especially cervical and colorectal cancer
- Discuss reproductive health
- Assess bone health
- Risk of vitamin D deficiency due to sun avoidance and decreased bone density from glucocorticoid use and inflammation
- Assess mental health
- Anxiety and depression is commonly seen in patients with lupus.
- Evaluate chronic pain when present and discuss interventions
Disease Overview & Diagnostic Workup
- Lupus is a complex multisystemic disease.
- Diagnosis is made clinically based on symptoms and signs.
- Use laboratory data to confirm the diagnosis.
- ANA is a hallmark of lupus but is not specific for lupus.
- Sun exposure can precipitate flares of lupus.
- Malar rash that spares the nasolabial fold is the most common lupus rash.
- Preventative health measures should be taken to prevent disease flares and complications.
Treatment
- Hydroxychloroquine is recommended for all patients with lupus.
- Dose is weight based
- Improves mortality
- Retinal screening recommended for long-term use of HCQ
- Choice of immunosuppressive therapies depends on organ involvement.
- Acute flares are often treated with a steroid taper, the length of which depends on the clinical manifestation(s).